Imagine a future where microscopic robots swim through your bloodstream, identify cancer cells before symptoms appear, and deliver medicine precisely where it’s needed—without surgery, without side effects. This isn’t science fiction. It’s the growing promise of nanotechnology in medicine.
As healthcare faces rising costs, aging populations, and a need for more personalized solutions, nanomedicine offers a powerful response. By working at the nanoscale (1 to 100 nanometers)—smaller than a red blood cell—these technologies can operate with unprecedented precision. But as with all medical revolutions, the path forward is both thrilling and ethically complex.
🔬 What Is Nanomedicine, Exactly?
Nanomedicine refers to the application of nanotechnology to diagnose, monitor, and treat disease. It includes:
-
Nanoparticles that can carry drugs directly to diseased cells
-
Quantum dots for real-time imaging of molecular processes
-
Nanosensors to monitor glucose, oxygen, or infections inside the body
-
Nanorobots designed to repair tissues or destroy harmful cells
These aren't just upgrades to existing tools—they represent a paradigm shift in how we understand and manipulate biology.
💉 Current Breakthroughs
1. Targeted Cancer Therapy
Instead of chemotherapy flooding the body, nanoparticles can deliver drugs only to tumor sites, reducing side effects and increasing effectiveness.
2. Smart Drug Delivery Systems
Responsive nanocarriers release medication only under specific conditions—like pH changes in infected tissue—creating more intelligent treatments.
3. Real-Time Biosensors
Injectable nanosensors are being explored to monitor heart health, detect early signs of sepsis, or manage chronic illnesses like diabetes from within the body.
🧩 Ethical and Regulatory Challenges
The rise of nanomedicine poses major questions:
-
Informed Consent: Will patients fully understand the risks of having invisible machines inside them?
-
Long-term Safety: How do we ensure nanoparticles don’t accumulate in organs or trigger immune reactions?
-
Data Privacy: Nanosensors could collect vast health data—who owns it, and who protects it?
-
Access Inequality: Will advanced nanomedicine be available to all—or just the wealthy?
⚖️ The Regulatory Gap
As with CRISPR and AI in healthcare, regulations lag behind innovation. Agencies like the FDA and EMA are developing new frameworks, but progress is slow, especially across borders.
🔮 What’s Next?
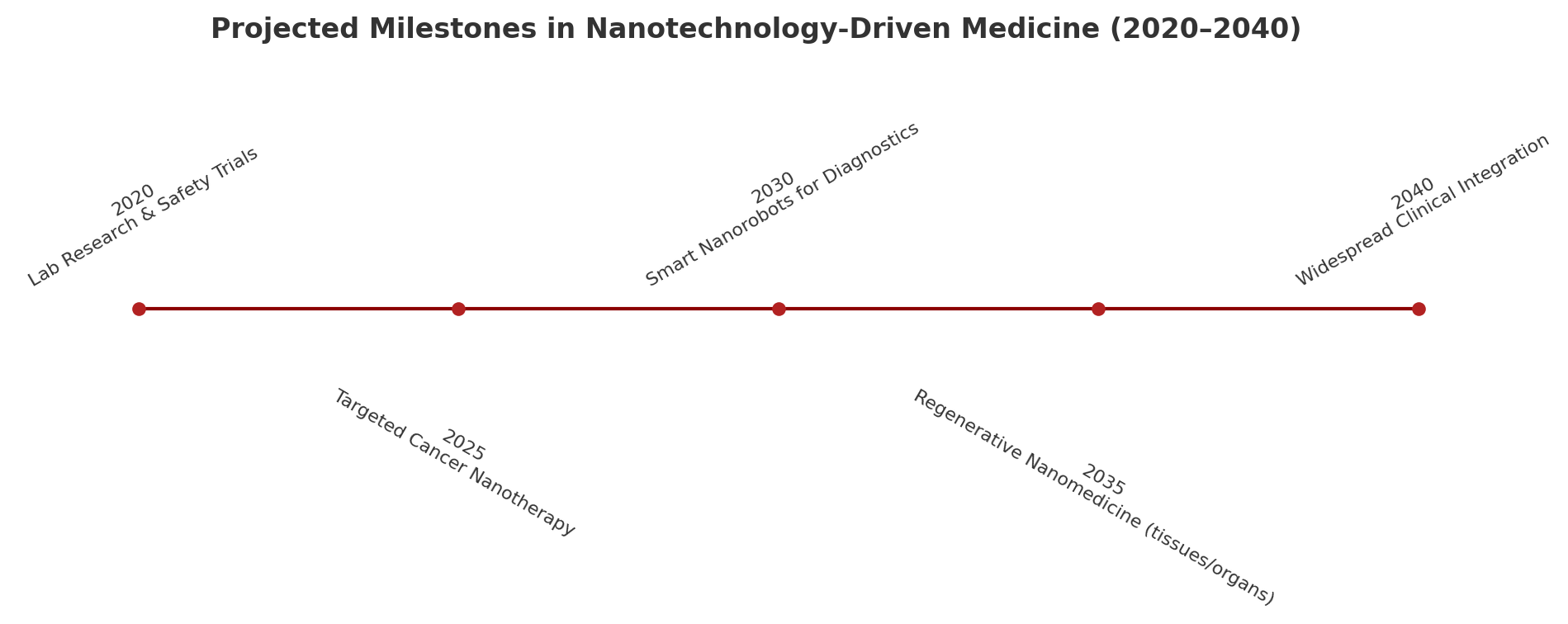
Looking ahead, experts forecast nanomedicine will become central to personalized healthcare by the 2030s. Possible breakthroughs include:
-
Nanofabricated tissues and organs for regenerative treatments
-
Neural nanotechnology for restoring vision or treating Parkinson’s
-
On-demand nanosurgery via magnetic or laser-guided devices
-
Smart implants that adapt in real time to biological signals
The combination of AI + nanotech may eventually allow continuous, invisible health monitoring—with intervention before illness ever manifests.
🧾 Conclusion: A New Era of Medicine, Molecule by Molecule
Nanotechnology won’t replace traditional medicine—but it will transform it. As we move from reactive to proactive care, and from generalized to hyper-personalized treatments, the smallest tools may bring the biggest healing.
The future of health could be measured in nanometers—but its impact will be immeasurable.
📰 Recent News & Developments + My Take
Here are several recent advances, trends, and challenges in nanomedicine (2024–2025), followed by my opinion as author.
🔬 Recent Advances & Trends
-
A new review highlights how nanotechnology is revolutionizing cancer immunotherapy — including strategies for combining drug delivery, immune activation, and targeting the tumor microenvironment.
-
Researchers emphasize that structure matters — carefully engineered spatial arrangement of nanomedicine components (antigens, adjuvants, surface ligands) can dramatically influence efficacy, targeting, and safety.
-
AI + nanomedicine are being integrated: one project used nanoparticles + AI and causality analysis to detect rare biomarkers in blood for metastatic prostate cancer and atherosclerosis.
-
Advances in drug delivery: for example, new lipid nanoparticle systems are being engineered for mRNA or gene editing payloads, with improved targeting, reduced toxicity, and better tissue specificity.
-
In more applied settings: researchers recently augmented vinegar’s antibacterial properties by combining carbon/cobalt nanoparticles, creating a non-toxic antimicrobial candidate.
-
In cancer therapy, nanotechnology is being used to deliver cisplatin in more precise and less toxic ways (e.g. polymeric, lipid, inorganic nanoparticles) to head & neck cancers.
-
In materials side, the DNA origami / nanostructure space is growing — programmable and modular nanosystems (for scaffolding, delivery, sensors) are being pushed further.
🧠 My Perspective (as Author)
I feel that nanomedicine is one of the most exciting frontiers in healthcare today — but we must temper excitement with prudence. A few of my thoughts:
-
Transformative potential is real. If we can truly deliver drugs at cellular precision, detect disease before symptoms, and intervene noninvasively, the shift in outcomes (reduced toxicity, earlier cures, better chronic disease management) could be dramatic.
-
But hurdles remain steep: reproducibility, scalability, regulatory oversight, safety, delivery (getting nanoparticles to exactly the right site), and long-term effects. Many of the “proofs in mice” have not translated as expected in humans.
-
The integration of AI + nanotech is especially promising. Designing optimal nanosystems from the combinatorial space is a nightmare of parameters; AI can help pick promising structures (as seen in structural nanomedicine efforts). But we must remain wary of overfitting, black box design, and safety blind spots.
-
I worry about overpromising and hype cycles. Sometimes headlines leap ahead of clinical validation. If patients or funders become disillusioned, momentum could slow.
-
The inequality risk is acute. I fear a two-tier medical future: those who can afford nanotech therapies get early detection and minimal side effects, while others remain stuck with older, more toxic treatments.
-
I expect the next decade to be a hybrid era: nanomedicine will begin in niche, high-need areas (e.g. cancer, rare disease, neurological repair) where the benefit/risk justifies early adoption. Over time, safer, more robust platforms will gradually diffuse more widely.
-
As an author, I hope the field moves not only toward raw power, but toward responsible nanomedicine — where transparency, patient understanding, robust safety pipelines, and equitable access are baked in from the start.
In conclusion: the future sketched by your original essay is plausible, and in many ways it's already beginning to take shape. But whether that future becomes a medical utopia or a cautionary tale will depend less on technology itself, and more on how wisely we deploy, regulate, explain, and democratize it.